Cardiology
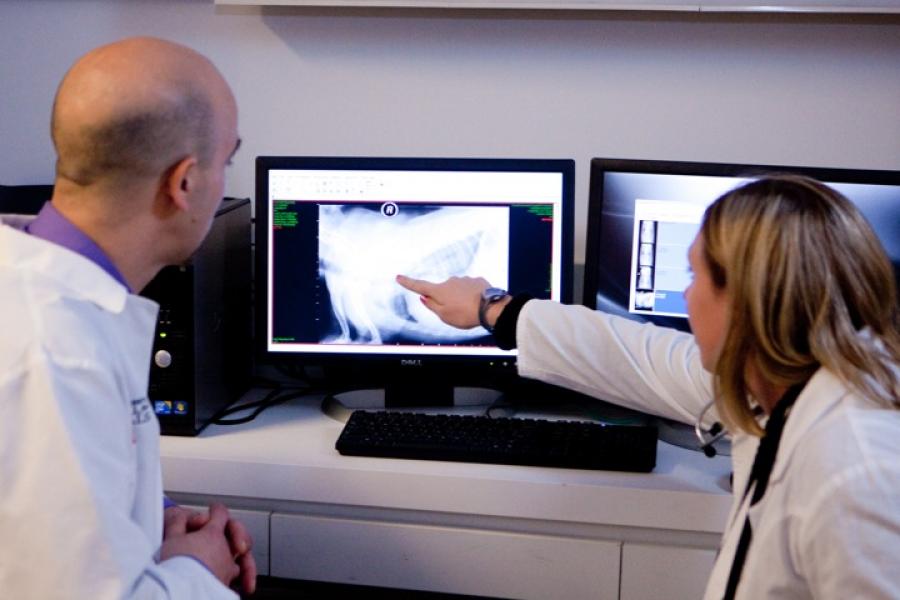
The clinical cardiology program at the Cornell University Hospital for Animals provides the most current diagnostic and treatment options for small animal patients. Local, national, and international collaborations with researchers and clinicians at Cornell and at other leading institutions have improved patient care in the field of veterinary cardiology and continue to keep our service at the forefront of the diagnosis and treatment of heart disease in companion animals.
 The Cardiology Service offers dedicated consultations and treatment in our state-of-the art facility. The most advanced diagnostics in veterinary medicine are provided, including echocardiography, electrocardiography, radiography, 24-hour electrocardiographic monitoring (Holter monitoring), laboratory work, and angiocardiography. In addition to the most current medical therapies, our service provides a number of interventional therapies including, but not limited to, pacemaker implantation, occlusion of patent ductus arteriosus, balloon valvuloplasty for pulmonic and subaortic stenosis, cardioversion of atrial fibrillation and radiofrequency catheter ablation of arrhythmias.
The Cardiology Service offers dedicated consultations and treatment in our state-of-the art facility. The most advanced diagnostics in veterinary medicine are provided, including echocardiography, electrocardiography, radiography, 24-hour electrocardiographic monitoring (Holter monitoring), laboratory work, and angiocardiography. In addition to the most current medical therapies, our service provides a number of interventional therapies including, but not limited to, pacemaker implantation, occlusion of patent ductus arteriosus, balloon valvuloplasty for pulmonic and subaortic stenosis, cardioversion of atrial fibrillation and radiofrequency catheter ablation of arrhythmias.
In the day to day care of patients in our hospital, we are keenly aware of the owners' concern for their pet, and we give our full attention to each person and animal that we are fortunate enough to meet. Moreover, we respect the fact that our clients have often taken time from their lives to drive a long distance to give to their animals the best care and we will do everything we can to meet and exceed these expectations.
News
-
Tiny dog’s big heart procedure is first of its kind at Cornell
-
A tale of two hearts: Mini Dachshund responds to novel treatment for dangerous arrhythmia
-
Cornell cardiologists publish new text on diagnosing arrhythmias
-
Careful cardiology approach returns feline arrhythmia patient to full health
-
Cornell veterinarians perform rare procedure to cure puppy's cardiac condition
-
Medicine without borders: Cornell cardiologists travel the world to improve treatment at home and abroad
-
Cardiology team saves street dog from deadly heartworm condition
What to Expect During Your Appointment
 Your scheduled visit to the Cardiology Service at the Cornell University Hospital for Animals begins with check in at the reception desk. You will be greeted in the waiting room by one or two students currently on their Cardiology rotation.
Your scheduled visit to the Cardiology Service at the Cornell University Hospital for Animals begins with check in at the reception desk. You will be greeted in the waiting room by one or two students currently on their Cardiology rotation.
The student(s) will then inquire about your pet's history and perform a physical examination of your pet. This experience is invaluable to the education and development of our students, and we appreciate your patience and understanding in allowing these future veterinarians to interact with you and your pet.
 The student(s) will then excuse themselves and consult with either a cardiology resident or cardiologist on service regarding their recorded history, physical examination findings, and recommendations for case management. A cardiologist or cardiology resident will then examine your pet and discuss their initial findings and recommendations for management of your pet's case.
The student(s) will then excuse themselves and consult with either a cardiology resident or cardiologist on service regarding their recorded history, physical examination findings, and recommendations for case management. A cardiologist or cardiology resident will then examine your pet and discuss their initial findings and recommendations for management of your pet's case.
In most cases, you will be asked to leave your pet in the care of the student(s) after this initial examination so that we may begin appropriate diagnostic testing, which commonly includes: electrocardiography, echocardiography, thoracic radiography, and noninvasive blood pressure measurement.
 Given our busy schedule and requisite interaction with other services in the care of your pet, you will most commonly be asked to return to discuss our findings and recommendations in the afternoon. Please understand that our primary concern is the well being of your pet, and that although we will always strive to minimize the duration of your stay, we do not wish to compromise patient care, and this may take some time. If minimal diagnostics are required, we may be able to significantly shorten the duration of your visit.
Given our busy schedule and requisite interaction with other services in the care of your pet, you will most commonly be asked to return to discuss our findings and recommendations in the afternoon. Please understand that our primary concern is the well being of your pet, and that although we will always strive to minimize the duration of your stay, we do not wish to compromise patient care, and this may take some time. If minimal diagnostics are required, we may be able to significantly shorten the duration of your visit.
 When you return to pick up your pet, you will meet with the cardiologist/cardiology resident and the student(s) who received you and your pet and discuss their findings and therapeutic recommendations (if any). In most cases, therapy will be in the form of medication that you can administer at home. In some cases, your pet may require hospitalization for supportive care and/or diagnostics, and the rationale and logistics of this recommendation will be discussed in depth upon your return. In the event that your pet requires an elective interventional procedure, the rationale, logistics, and risks associated with the procedure will be discussed at this time, and the procedure can often be scheduled either at the time of discharge or within 24 hours of discharge.
When you return to pick up your pet, you will meet with the cardiologist/cardiology resident and the student(s) who received you and your pet and discuss their findings and therapeutic recommendations (if any). In most cases, therapy will be in the form of medication that you can administer at home. In some cases, your pet may require hospitalization for supportive care and/or diagnostics, and the rationale and logistics of this recommendation will be discussed in depth upon your return. In the event that your pet requires an elective interventional procedure, the rationale, logistics, and risks associated with the procedure will be discussed at this time, and the procedure can often be scheduled either at the time of discharge or within 24 hours of discharge.
 Prior to your leaving the Hospital, you will receive a copy of the cardiology report, which outlines the findings and recommendations for management of your pet's case using some medical terminology that you may not be familiar with. Your referring veterinarian (who will be more familiar with terminology used) will also receive a copy of this report via mail. You will also receive a copy of discharge instructions, which outlines our findings and recommendations in more vernacular terms, and we will strive to make sure that we have answered any and all questions that you may have prior to your departure.
Prior to your leaving the Hospital, you will receive a copy of the cardiology report, which outlines the findings and recommendations for management of your pet's case using some medical terminology that you may not be familiar with. Your referring veterinarian (who will be more familiar with terminology used) will also receive a copy of this report via mail. You will also receive a copy of discharge instructions, which outlines our findings and recommendations in more vernacular terms, and we will strive to make sure that we have answered any and all questions that you may have prior to your departure.
Medical Conditions
|
|
Arrhythmia Mapping and Ablation
Cardiac mapping and ablation (also called catheter ablation; radiofrequency ablation) is a procedure used to diagnose and treat abnormal heart rhythms (arrhythmias). It consists in finding (mapping) the precise location of the source of the arrhythmia with catheters that are threaded through blood vessels and guided into various areas of the cardiac chambers. The abnormal heart tissue is then destroyed (ablated) using radiofrequency energy (heat).
 This technique is used to treat arrhythmias that cause rapid heart rates. It is an alternative to antiarrhythmic drugs, when these medications fail to control an arrhythmia or when they are associated with side-effects. Catheter ablation can be curative.
This technique is used to treat arrhythmias that cause rapid heart rates. It is an alternative to antiarrhythmic drugs, when these medications fail to control an arrhythmia or when they are associated with side-effects. Catheter ablation can be curative.
How do I know that my pet is a candidate for an ablation procedure?
Currently cardiac ablation is only performed in dogs. Dogs with arrhythmias that can be treated with this procedure might experience episodes of weakness or fainting, exercise intolerance and extended periods of panting, and even heart failure. Because not all arrhythmias can be treated via cardiac ablation, several diagnostic tests, performed by a board-certified cardiologist are necessary to determine if your pet is a candidate.
Which arrhythmias are treatable with cardiac ablation?
The arrhythmias that are treatable with this procedure are called tachycardia because they are responsible for rapid heart rates, on occasion above 300 beats/minute. Most of these tachycardias originate from the upper portion of the heart, above the ventricles, and are called supraventricular tachycardias. They include: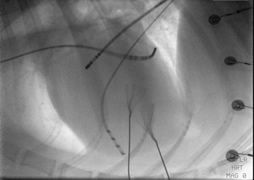
-
Accessory pathway-mediated tachycardia (atrioventricular orthodromic reciprocating tachycardia)
- Common in Labradors and Boxers
- >90% success rate with ablation
-
Focal atrial tachycardia
- 55% to 60% success rate with ablation
-
Atrial flutter
- Common in Bernese Mountain dogs and Dogue de Bordeaux
- 60% to 95% success rate depending on the type of atrial flutter
- Persistent atrial fibrillation
Some specific forms of ventricular tachycardia, that occur in English bulldogs, can be treated with cardiac ablation.
Which tests are required to determine if my dog can be treated with this technique?
In order to determine if your pet can benefit from cardiac ablation, the following tests need to be performed:
- An electrocardiogram (12-lead ECG)
- An echocardiogram, which is an ultrasound of the heart
- A 24-hour Holter, which is a 24-hour recording of an ECG
- Blood tests
What should I expect when I bring my dog to Cornell?
Your pet will usually be hospitalized the day before and will be able to go home the day after the procedure. Blood tests will usually be performed at the time of admission. The day of the procedure, your dog will be placed under general anesthesia and hair will be clipped in various areas of his body. Catheters will be inserted into veins from the neck and groin regions. Continuous X-ray imaging, called fluoroscopy, will be used to guide the catheters into various areas of the cardiac chambers. Once in place, the catheters will be used to record the electrical activity of the heart and trigger the arrhythmia using specialized equipment. Finally, radiofrequency energy will be delivered from a catheter where the arrhythmia is originating from to destroy the abnormal heart tissue. The procedure takes 3 to 4 hours. Your dog’s recovery will be monitored overnight in the intensive care unit.
 Are there risks associated with this procedure?
Are there risks associated with this procedure?
Cardiac ablation is generally safe. We will discuss with you some rare complications:
- Bleeding where the catheters are inserted
- Anesthetic complications, adverse drug reactions
- Fluid around the heart (cardiac tamponade)
- Damage to the normal cardiac electrical conduction system, causing slow heart rate (bradycardia) and requiring pacemaker implantation
- Damage to the heart valves, walls and large vessels
- Ventricular fibrillation
Are rechecks needed after the procedure?
In order to confirm that the ablation was successful, we recommend that you bring your pet back to Cornell for a recheck evaluation approximately 1 month after the procedure. An echocardiogram, a 12-lead ECG and a 24-hour Holter are performed at the time of the visit. If it is not possible for you to come back to Cornell, these tests can also be done by your local board-certified cardiologist, who will share the results with us.
When can cardiac ablation be performed on my pet?
We are currently not able to perform cardiac ablations year-round. Call for current availability.
Always have your veterinarian first contact us before referring you and your dog to the cardiology service at Cornell University Hospital for Animals for an ablation procedure.
Holter Monitoring
Holter monitoring is a noninvasive method of assessing the heart's rhythm and rate. It is a 24-hour electrocardiogram that is recorded while the animal is "wearing" a recorder. This permits an analysis of the rhythm and rate of the heart throughout the day and night of the dog with activities documented in a diary by the owner. Your veterinarian may recommend this diagnostic procedure for the following reasons:
- an arrhythmia is suspected in your pet
- your pet exhibits signs of weakness, dizziness, lethargy, excessive panting and agitation, or even collapse or fainting episodes
- to monitor drug therapy and effects on the heart rate and rhythm
- to monitor programming effects if your pet has an implanted pacemaker
 After clipping away some fur and cleansing the skin, several electrode patches are adhered to the skin over the right and left chest areas and along the sternum. The Holter monitor is a small digital unit with a main cable and 7 wires. The wires snap onto the electrode patches. It is then wrapped up with soft bandage materials around your pet’s ribcage. If an appropriately sized vest is available, your pet will be outfitted with a vest over the wrap.
After clipping away some fur and cleansing the skin, several electrode patches are adhered to the skin over the right and left chest areas and along the sternum. The Holter monitor is a small digital unit with a main cable and 7 wires. The wires snap onto the electrode patches. It is then wrapped up with soft bandage materials around your pet’s ribcage. If an appropriately sized vest is available, your pet will be outfitted with a vest over the wrap.
The technician will communicate with you on the removal procedure. A daily log will be your homework. Recording your pet's activities during the 24 hours is extremely important and will help correlate daily activity with the heart's rhythm and rate. The ECG data is not sent out to a human medicine lab but is meticulously edited by our cardiology technical staff and reviewed and interpreted by the clinicians who will make therapy recommendations based upon the results.
Cardiology Related Information
American College of Veterinary Internal Medicine
A non-profit board created to enhance animal and human health by advancing veterinary internal medicine through training, education, and discovery.


 Are there risks associated with this procedure?
Are there risks associated with this procedure?